Transfusion medicine
Transfusion medicine handbook
The Transfusion Medicine Handbook is designed to assist hospital staff and other health professionals in modern Transfusion Medicine Practice.
6. Special Circumstances
6.9 Avoidable Haemostatic Problems in Elective Surgery
Any patient planned for elective surgery must be asked about previous episodes of abnormal bleeding. Underlying medical conditions, medication associated with impaired haemostatic function, or abnormal coagulation test results may require postponement of surgery until the abnormality has been identified or confirmed. Appropriate procedures should be undertaken prior to surgery to minimise the perioperative risks for bleeding and/ or thromboembolism. This may include consultation with specialists.
Congenital abnormalities of haemostasis such as haemophilia should be managed in consultation with a specialist haemophilia centre.
Warfarin
Unless contraindicated, warfarin anticoagulation should be stopped early enough before elective surgery to allow the prothrombin time (or INR; International Normalised Ratio) to approach normal. This should be guided by a local protocol for preoperative anticoagulant management, considering patient-related risk factors for both thrombosis and bleeding. Bridging anticoagulation with either low molecular weight heparin or heparin infusion may be indicated for patients with at least a moderate risk of thrombosis. Prior to surgery where the INR is stable and therapeutic, withdrawal of warfarin for 3 - 5 days is generally adequate to achieve reversal sufficient for surgery. A longer period may be required in the presence of malnutrition or other factors predisposing to vitamin K deficiency.
The Thrombosis & Haemostasis Society of Australia and New Zealand (THANZ) provides a guideline for warfarin reversal [7]. The consensus guidelines contain recommendations for the management of patients on long-term warfarin undergoing invasive procedures.
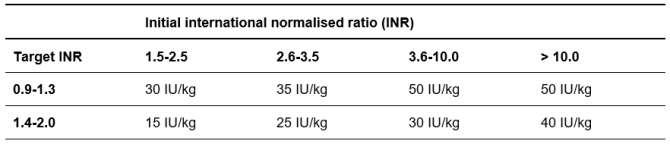
Additionally, guidance for managing patients undergoing elective and emergency surgery, including urgent reversal using Prothrombinex-VF, a three-factor prothrombin complex concentrate (3FPCC), is available via the NZBS Reversing Warfarin app developed by HealthObs Ltd (available for Android and iPhone). In the setting of four-factor PCCs, the NZBS Anticoagulation Reversal webpage and the NZBS Warfarin Reversal using Beriplex NZ leaflet will be made available when Beriplex NZ (4FPCC) is introduced into New Zealand hospitals during 2025. Guidance on 4FPCC use prior to surgery is available in Table 6.3.
Table 6.3: Urgent Warfarin reversal in non-bleeding patients using a four-factor PCC, e.g. prior to surgery
Outside of the peri-operative setting, 4FPCC use should only be considered if INR >10 and there is a high risk of bleeding.
In patients > 100 kg, the dose of BERIPLEX NZ is calculated based on a capped 100 kg body weight and maximum dose of 50 IU/kg (i.e., the maximum absolute dose is 5000 IU).
Source: Updated recommendations for warfarin reversal in the setting of four-factor prothrombin complex concentrate (2024) on behalf of the Thrombosis & Haemostasis society of Australia and New Zealand (THANZ).
©The Medical Journal of Australia – reproduced with permission
Non-Vitamin K-Dependent Oral Anticoagulants (DOAC)
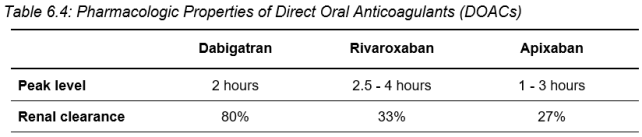
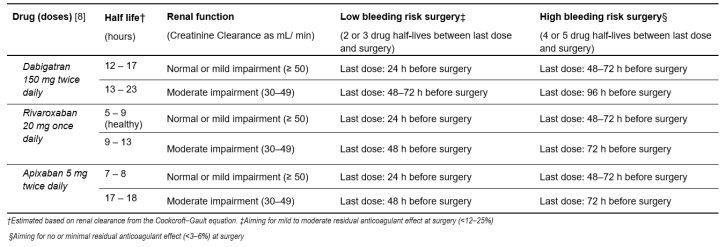
Direct thrombin inhibitors, such as dabigatran (Pradaxa), and direct Factor Xa inhibitors, such as rivaroxaban (Xarelto) and apixiban (Eliquis), are non-vitamin K-dependent oral anticoagulants. They should be stopped early enough before elective surgery to allow reversal of the anticoagulant effect. This should be guided by a local protocol for preoperative anticoagulant management. In the case of dabigatran, the patient's renal function is particularly important. Guidance from the ASTH and PHARMAC is available [7] [8]. For further information see Table 6.4: Pharmacologic Properties of DOACs and Table 6.5: Preoperative interruption of new oral anticoagulants: a suggested management approach.
Additionally, the Rivaroxaban app and the Dabigatran app developed by Health Obs Ltd, available for Android and iPhone, provide guidance for managing patients undergoing elective and emergency surgery.
Table 6.4: Pharmacologic Properties of Direct Oral Anticoagulants (DOACs)
Table 6.5: Preoperative interruption of new oral anticoagulants: a suggested management approach
Aspirin
The antiplatelet effect of aspirin is mediated via irreversible acetylation of platelet cyclo-oxygenase, specifically COX-1, and the resulting inhibition of thromboxane A2 synthesis. Aspirin is indicated for the management of ischaemic atherosclerotic vascular disease including coronary artery and cerebrovascular disease and is used primarily in secondary prevention. Aspirin is used in combination with ADP-receptor inhibitors for the management of acute coronary syndromes (ACS) and for thromboprophylaxis following stent implantation.
It may also be used for the management of some rheumatological disorders. While a single 75 mg dose of aspirin may impair platelet function for several days, the effect is less than with newer antiplatelet agents and most surgery can be performed after discontinuing aspirin at most the day prior to surgery. Prior to neurosurgery, transurethral prostatectomy or other invasive procedures with a major risk of bleeding or complications from bleeding, aspirin should (unless contraindicated) be stopped 3 days before planned surgery.
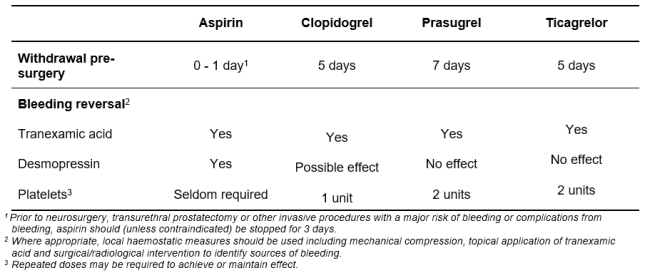
If aspirin-induced platelet defect contributes to abnormal bleeding, desmopressin and tranexamic acid are likely to be effective in controlling haemostasis. Refer to Section 8.5: Desmopressin and Section 8.6: Tranexamic Acid for further information on these agents including dosing guidelines. Platelet transfusion is seldom necessary.
Non-steroidal Anti-inflammatory Drugs (NSAID)
Non-steroidal anti-inflammatory drugs cause reversible, but non-selective, inhibition of cyclo-oxygenase, both COX-1 and COX-2. The effects usually last for hours, as opposed to lasting days with aspirin. Normal platelet function is usually rapidly restored once the NSAID is stopped. The length of time that these medications should be stopped prior to an invasive procedure varies as the antiplatelet effect is dependent on the half-life of the NSAID being used. If NSAID-induced platelet defect contributes to abnormal bleeding, desmopressin and tranexamic acid may be effective in controlling haemostasis. Platelet transfusion is seldom necessary. The effect of both desmopressin and platelet transfusion will be reduced in the presence of active drug.
P2Y12 Adenosine Diphosphate (ADP) Receptor Inhibitors
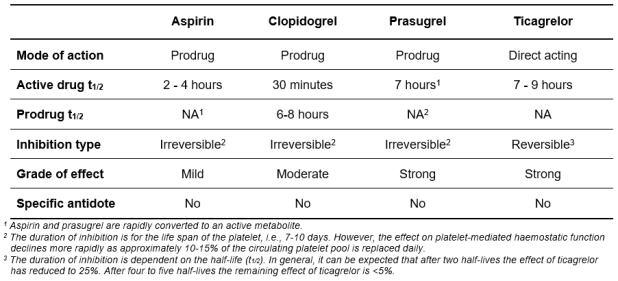
Clopidogrel and the other thienopyridines, and ticlopidine, irreversibly inhibit the P2Y12 subtype of ADP receptor on platelet cell membranes. Ticagrelor (Brilinta), reversibly inhibits the P2Y12 ADP receptor. See Table 6.6: Pharmacologic Properties of Anti-Platelet Agents
Clopidogrel is indicated for the management of ischaemic atherosclerotic vascular disease including coronary artery and cerebrovascular disease. Ticagrelor are indicated for the management of acute coronary syndromes (ACS) and as prophylaxis against stent thrombosis, usually in combination with aspirin. P2Y12 ADP receptor inhibitors should be used with caution in patients at increased risk of bleeding such as in the setting of trauma, surgery or other pathological conditions of haemostasis. Unless contraindicated, clopidogrel should be discontinued at least 5 days prior to surgery where an anti-platelet effect is undesirable.
Ticagrelor, although reversible, has a pronounced effect on platelet function and should be discontinued at least 3 days prior to semi-urgent surgery and 5 days prior to elective surgery. If P2Y12 ADP receptor-induced platelet defect contributes to abnormal bleeding, tranexamic acid together with a 1 - 2 unit platelet transfusion is likely to be effective in controlling haemostasis. Ticagrelor has a long half-life and inhibition of even transfused platelets may occur. See Table 6.7: Managing Bleeding in Patients on Anti-Platelet Agents
In patients with ACS who have recently received a coronary stent, platelet transfusion carries a risk of arterial and stent thrombosis and should therefore be restricted to situations involving serious bleeding or high bleeding risk.
Platelet Glycoprotein IIb (GPIIb) and IIIa (GPIIIa) Inhibitors
The platelet glycoproteins GPIIb and GPIIIa have important roles in normal haemostasis and pathological thrombosis. The peptides tirofiban (Aggrastat) and eptifibatide (Integrilin) inhibit GPIIb and GPIIIa receptors. The supply of abciximab (REOPRO) has been discontinued in New Zealand.
Tirofiban and eptifibatide bind reversibly to GPIIb/IIIa receptors and the antiplatelet effect usually recovers within 4 - 8 hours following cessation of treatment. It should be noted that tirofiban not been approved for use in New Zealand [9] and as such may only be supplied under Section 29.
Table 6.6: Pharmacologic Properties of Anti-Platelet Agents
Table 6.7: Managing Bleeding in Patients on Anti-Platelet Agents