Transfusion medicine
Transfusion medicine handbook
The Transfusion Medicine Handbook is designed to assist hospital staff and other health professionals in modern Transfusion Medicine Practice.
6. Special Circumstances
6.16 Transfusion of the Newborn
Red Cells
Normal blood volume at birth varies according to gestational age and timing of clamping of the cord. For term infants the average blood volume is 80 mL/kg whilst in pre-term infants it is higher at 106 mL/kg. The newborn bone marrow does not respond as rapidly as an adult’s and any uncorrected blood loss can rapidly lead to anaemia.
Common indications for transfusion are:
- Anaemia of Prematurity: This is common in the very preterm baby and is caused by delayed red cell production from an immature bone marrow and iatrogenic blood loss from repeated sampling
- Anaemia related to problems in utero: Fetal anaemia can be due to non-haemolytic causes such as fetomaternal haemorrhage and twin anaemia polycythaemia syndrome or red cell production problems such as Parvovirus infection or Diamond Blackfan Syndrome (primary red cell aplasia) [16].
The volume of red cells to be transfused in newborns depends on the weight and local policy. A typical volume for top-up transfusion is 10 - 20 mL/kg at an infusion rate of 5 mL/kg/hr. Top-up transfusions in excess of 20 mL/kg are not recommended because of the risk of transfusion-associated circulatory overload (TACO) [17]. Frusemide given at a dose of 1 mg/kg halfway through the transfusion may sometimes be required to minimise volume load.
Some centres prefer to limit donor exposure in newborns. NZBS provides small volume ‘neonatal’ red cell units which are produced by separating an adult ‘plasma-reduced’ red cell donation into several equal-sized aliquots. All (or some) of the individual aliquots from one adult unit can be reserved for sequential transfusions to the same baby over the full 35-day shelf life of the red cells.
Compatibility Testing
The normal rules for ABO and RhD compatibility apply. However, for infants 4 months of age or under, maternal blood may be used for pretransfusion testing provided the ABO groups of mother and infant are compatible since any clinically significant red cell antibody present in the infant's circulation will have come from the mother. Blood components selected for transfusion should be compatible with any ABO or other red cell antibody present in the maternal or infant plasma. Repeated transfusions during the infant’s first 4 months of life do not require further compatibility testing if there are no atypical maternal red cell antibodies in the maternal or infant plasma. However, if the antibody screen is positive, full pretransfusion testing and crossmatch will be necessary.
Pretransfusion testing of infants 4 months or older should be performed on a sample from the infant.
Exchange Transfusion
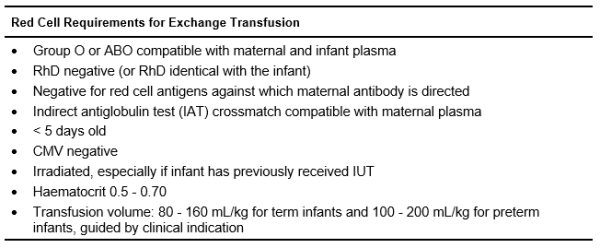
For severe cases of HDFN, neonatal exchange transfusion may be required. Table 6.13 shows the requirements for red cells used in this procedure.
Table 6.13: Red Cell Component Requirements for Neonatal Exchange Transfusion